
A Novel Approach to Mitigate the Opioid Overdose Epidemic: The OCRM Model January 04, 2022
Tens
of thousands of people in the United States lose their lives each year to drug
overdose, and the numbers continue to mount. Since 1999, approximately 841,000 such
deaths occurred in the United States, while
the number of drug overdose deaths increased 120% between
2010 and 2018 and totaled nearly 70,630 per year by 2019.
During the COVID-19 pandemic, drug overdose deaths increased more than 20%
in 25 states and the District of Columbia. Worldwide
in 2019, around 36 million people suffered from drug use disorders.
Today,
overdose death is a leading cause of injury-related death in the United States.
To mitigate the opioid overdose epidemic, an evidence-based approach is needed and this approach should
· target and reduce opportunities for access to illicit drugs;
· use a collaborative multidisciplinary approach to improve
responses to overdose incidents; and
· have access to data for the development of mitigation strategies
and the evaluation of outcomes.
Reducing
the Accessibility of Opioids
Nearly
85% of drug overdose deaths involve illicit drugs such as fentanyl, heroin,
cocaine, and methamphetamine, according to a recent
study. Law enforcement efforts based on data from various resources are key
to reducing the accessibility of illicit drugs.
Research
has shown that a small number of prolific offenders control illicit drug
markets and that drug-sale locations form hot spots,
with a small number of addresses. Rigorous data analysis can help identify and
dismantle the network of prolific offenders in the drug-sale hot spots, which in
turn reduces the accessibility of opioids to experienced and novice drug users.
Collaborative
and Multidisciplinary Approach
Identifying
risk factors for drug overdose can lead to prevent overdose deaths. According
to a recent survey,
in more than 3 out of 5 overdose deaths, at least one potential opportunity to prevent
the death through life-saving strategies was found.
These
strategies include:
(1)
providing access
to health-care services, risk-reduction services, and the drug naloxone (to rapidly
reverse an opioid overdose);
(2)
focusing on prevention
of initial drug use; and
(3)
using multiple
drugs to treat substance-use addiction.
Indeed,
a collaborative and multidisciplinary approach is essential for the successful
implementation of these outreach strategies. For instance, a recent study examined collaborative
programs that involved local public health and public safety agencies in
Massachusetts. These programs aimed to help overdose survivors by connecting
them with harm-reduction and addiction-treatment services.
Through
online surveys and interviews with police and fire departments in 351
Massachusetts communities, the researchers were able to identify four types of effective
programs:
· multidisciplinary team visits (i.e., post-overdose visit to the
survivor to provide information and referrals for the survivor, the survivor’s family,
and the survivor’s associates),
· police visit (i.e., post-overdose visit to the survivor and to
provide a referral to public health services),
· clinician outreach (i.e., post-overdose telephone-based contact
with the survivor), and
· location-based outreach (i.e., media and word-of-mouth contact
with the entire community, including drug-overdose survivors).
These
outreach programs had in common the use of enhanced collaboration and
information sharing among stakeholders to identify drug users and the use of
timely and effective intervention efforts to prevent overdose deaths.
Access
to Data
Access
to reliable data is the key to success in an evidence-based policy. A recent study examined the
core elements of successful overdose prevention activities in four states
(Massachusetts, New Hampshire, New Mexico, and Utah) that managed to decrease
their high rate of opioid-involved overdose deaths from 2016 to 2017 through
the analysis of program narratives. The study found that access to drug-abuse
data, the capacity to analyze the data, and the ability to disseminate the
findings of the data analyses played vital roles in the four states’ successful
overdose-prevention strategies. The findings were systematically disseminated through
either web-based dashboards or quarterly reports. Drug-abuse prevention
organizations in partnership with members of the local community then used the
findings to create effective program models for the prevention of overdose
deaths.
The
Opioid Control and Reduction Model
To address the need for a novel and comprehensive approach to curbing the opioid overdose epidemic, we offer the Opioid Control and Reduction Model (OCRM), which is illustrated below. The OCRM suggests that comprehensive analysis of data from three sources (i.e., law enforcement, hospital emergency department, and pharmacies) can lead to successful collaborative outreach programs aimed at controlling the rise in and ultimately reducing overdose deaths and increasing the ability of law enforcement officials to identify prolific drug offenders.
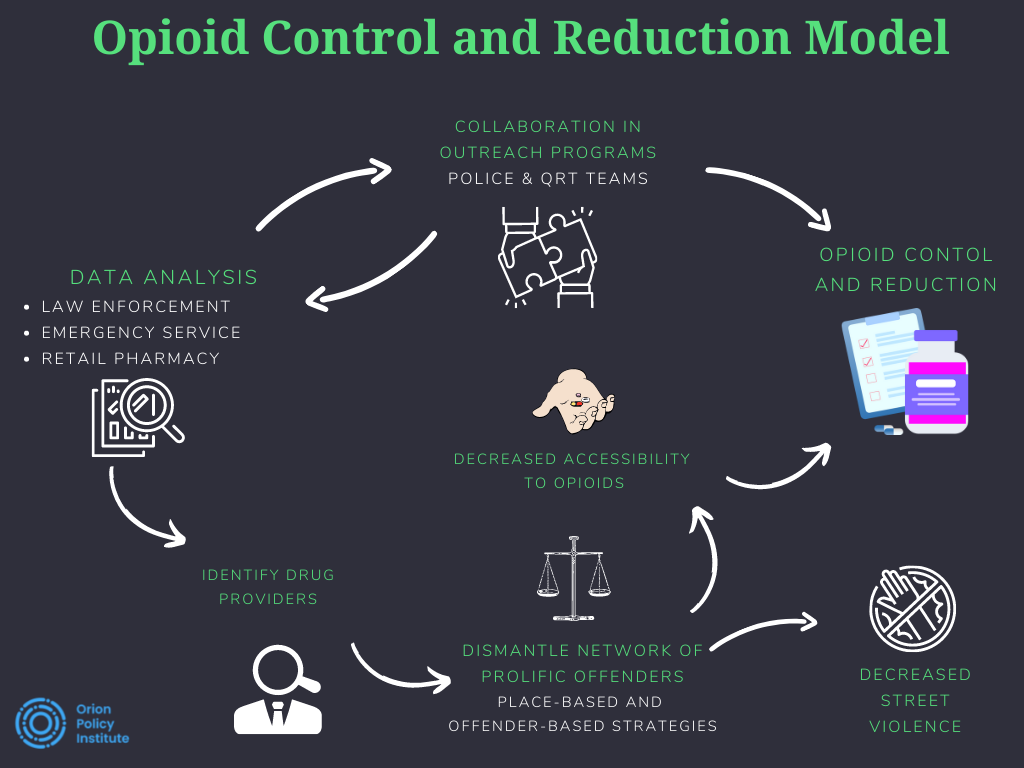
The
OCRM involves three steps:
(1) data analysis,
(2) identification and dismantling of illicit drug networks, and
(3)
development of
outreach-program quick-response teams.
Step
1: Data Analysis
The
first step in the model is data analysis from at least three sources: law
enforcement, hospital emergency departments, and pharmacies.
Law
Enforcement Data
The
proposed model analyzes law enforcement data to identify a small number of
prolific offenders who control the drug markets. Studies have found that
most gang members and prolific offenders sell illegal drugs as their primary
source of income. These same individuals also are the primary instigators of
street violence. A recent
study showed that overdose victims are connected to gang members and to prolific
offenders who sell drugs in a mutually beneficial, and sometimes
confrontational, cyclical relationship.
Spatial
analyses showed a close relationship between drug points of sale and other
criminal activities such as street robbery and prostitution. Place-based and
offender-based policing techniques, can be used to limit access to opioids,
reduce street violence, and dismantle the illicit drug network, thereby reducing
the number of overdose deaths.
Hospital
Emergency Department Data
The
OCRM also uses data from hospital emergency departments to increase the
accuracy of information about police contacts with opioid users and identify
individuals who need treatment and the support of an OCRM quick response teams.
For example, when both sets of data identify an individual with a history of
drug abuse, the police are notified and an OCRM quick response team contacts
the individual to provide proactive intervention to reduce the chances of an opioid
overdose and decrease the demand and market for the illicit drug.
Retail
Pharmacy Data
The
elimination of illicit drug networks alone may not be adequate to control the
spread of opioids. Retail pharmacy data can be used to identify individuals who
abuse their access to opioids intended for legitimate medical purposes. The
analysis of the pharmacy data provides an opportunity to control the
introduction and circulation of a medically legitimate drug for illicit
purposes in the community.
Step
2: Identification and Dismantling of Illicit Drug Networks
A
comprehensive analysis of data from the three sources (i.e., police, hospital
emergency departments, and pharmacies) will help the police to identify prolific
offenders and dismantle illicit drug-sale networks, leading to two positive
outcomes.
First,
the accessibility of illicit drugs will be reduced for experienced and novice
users.
Second,
the overall crime rate and the extent of crime victimization will drop because
the violent and property crimes typically associated with illicit drug markets
will be reduced.
Step
3: Development of Outreach-Program Quick-Response Teams
The
final step in the model calls for police to contact opioid users, gauge the
users’ likelihood of overdosing, and provide the users with information about
treatment options available in the community. A recent
study in Cincinnati found that such contacts enable police to predict at
least 10% of overdose victims before they overdose.
Current
law enforcement practices for dealing with drug users typically involve arrests
or citations. Under the OCRM, information obtained from police contacts with
drug users can lead to the development of proactive and collaborative measures
to prevent overdose deaths.
To
achieve these outcomes, police must analyze the data obtained from their
contacts with drug users and share the findings about potential drug-overdose
victims with quick response teams (QRTs) that consist of police, firefighters,
and addiction specialists.
QRTs
are “pre-arrest diversion (deflection) programs that involve interdisciplinary
overdose follow-up and engagement with survivors to link individuals to
treatment during the critical period following overdose.” QRTs
originated in Colerain Township, Ohio, and spread to communities across the
country that have suffered significantly from opioid overdoses and overdose
deaths.
QRTs
play a vital role in the OCRM because the teams focus on providing opioid users
with treatment options rather than seeking to arrest and label them as
criminals. The information obtained from these interactions can help state
governments to better understand the scope of the overdose problem in their jurisdiction
and develop programs that can prevent overdoses and thus prevent overdose
deaths.
The
QRTs also collect opioids users’ data on various aspects of drug abuse, such as
how the individual started using opioids, whether the individual’s friends use
opioids, how the individual acquires opioids, and what kind of opioids the
individual uses. The information is then added to the database pool for daily
analysis and a better understanding of the extent of the opioid problem in real-time.
Policy
Recommendations
We
provide the following recommendations for a successful implementation of the
OCRM:
· All stakeholders (i.e., policymakers, police, fire departments,
health-care systems, addiction professionals, and pharmacies) must be committed
to contributing to this model through ongoing communication, information
sharing, and the provision of necessary resources.
· For enhanced collaboration, the stakeholders must meet regularly to
discuss the needs of stakeholders that adopt the OCRM and the challenges that first
responders face when implementing the model.
· An oversight committee must be established with the involvement of
policymakers and management representatives given responsibility for providing solutions
to challenges that arise for one or more stakeholders.
· The roles and responsibilities for data sharing, data analyses,
and the QRTs should be clearly identified and communicated to all partners
through a program manual.
· Data-sharing agreements should be signed by all OCRM partners to
ensure that the necessary data are included in the databases and that comprehensive
data analyses are conducted to guide QRT outreach efforts and law enforcement
tasks related to opioid users and opioid overdoses.
· Data-sharing
agreements and protocols should clearly describe data-use guidelines,
including:
o
prohibitions
against use of the data in its raw form or the results of the analyzed data in any
way that could lead to adverse consequences for persons named in the database,
such as eviction, stigmatization, and social control;
o
protection of
privacy rights and consequences for violations of those rights;
o
the use of unclear
descriptions of data sharing processes that might deter individuals at highest
risk for overdose from calling for emergency assistance.
A
formal program evaluation must be conducted on a regular basis (e.g.,
annually). Such evaluations should include an evaluation of outcomes through quantitative
and qualitative research methods. Modifications to how the model is implemented
should be made as deemed appropriate at the end of the program-evaluation
process.
Systematic reviews and meta-analyses of the OCRM as implemented must be conducted to ensure that the model is effective in mitigating the opioid overdose epidemic.
______________________________________________________
Orion Policy Institute (OPI) is an independent, non-profit, tax-exempt think tank focusing on a broad range of issues at the local, national, and global levels. OPI does not take institutional policy positions. Accordingly, all views, positions, and conclusions represented herein should be understood to be solely those of the author(s) and do not necessarily reflect the views of OPI.
_________________
Dr. Murat Ozer is an Assistant Professor at the School of IT, University of Cincinnati. He is a crime analyst and cybersecurity lecturer. He also works with Cincinnati Police Department and develops certain web-based predictive analytical systems. His research interests are primarily in managing big data sources of law enforcement agencies to generate predictive data analytics for various public health problems such as gun violence, and opioid overdoses. He is also co-founder of Peel9, a record management system and data analytics company.
Professor John Wright is a Professor at the Criminal Justice Program, University of Cincinnati. He subsequently served five years on the faculty at East Tennessee State University. Dr. Wright’s work has sought to integrate findings from a number of disciplines, including human behavioral genetics, psychology, and biology. He has published over 200 articles and book chapters and was recently judged to be one of the most prolific and most-cited criminologists in the United States. Dr. Wright consults with states and local jurisdictions and is a much sought-after lecturer.
Dr. Davut Akca completed his Ph.D. degree in the Forensic Psychology program of Ontario Tech University. He worked as a Post-Doctoral Research Officer at the Centre for Forensic Behavioural Science and Justice Studies at the University of Saskatchewan and Dr. Davut Akca is currently an Assistant Professor at the Criminology program of Lakehead University, Orillia campus.
